RTM in 2026: The Compliance Pivot That Will Decide Who Wins (and Who Panics)
- Matthew Jurek
- Jan 16
- 4 min read
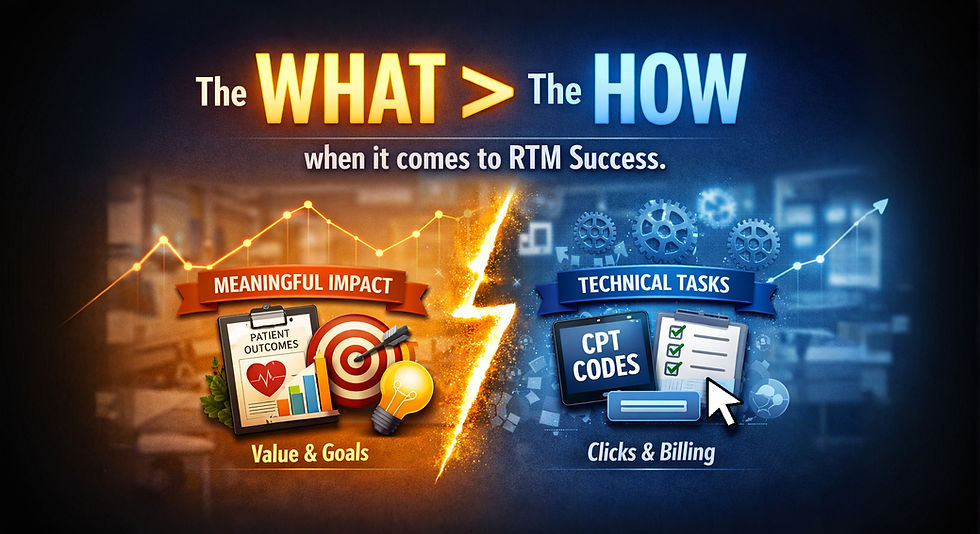
RTM Isn’t “Extra Revenue” Anymore — It’s a Clinical Test
For the last few years, the dominant RTM question was simple:“How can we bill for this?”
By 2026, CMS has quietly shifted the question to something far more consequential:“How are you justifying this?”
In the CY 2026 Medicare Physician Fee Schedule Final Rule, CMS expanded RTM billing flexibility by introducing codes that allow reimbursement for shorter data transmission windows (2–15 days) and shorter treatment management time (10–19 minutes). This change moves away from the rigid thresholds that previously excluded many clinically appropriate use cases.
That’s the good news.
The less-talked-about part? CMS doubled down on the requirement that RTM services must be reasonable and necessary for the diagnosis or treatment of illness or injury. Minutes logged and devices connected do not, by themselves, establish medical necessity.Source: Centers for Medicare & Medicaid Services (CMS), CY 2026 Medicare Physician Fee Schedule Final Rule – cms.gov
In other words, RTM is no longer about whether activity occurred. It’s about why it occurred and what changed because of it.

Shorter Billing Thresholds Don’t Lower the Bar — They Raise It
One of the most misunderstood aspects of the 2026 RTM updates is the assumption that expanded codes make RTM easier.
They don’t.
They make workflow weaknesses more visible.
Industry analyses highlight that shorter billing thresholds allow clinics to capture legitimate care episodes that previously went unreimbursed—post-op transitions, short flare-ups, adherence monitoring, and functional regressions.
But when monitoring windows shrink, documentation clarity becomes critical. Clinics can no longer rely on vague notes or templated language. The clinical narrative has to clearly connect:
the patient’s condition
the data reviewed
the clinical interpretation
the resulting action or decision
RTM doesn’t create more work. It reveals whether your work is intentional or informal.
RTM Makes Invisible Care Visible
One of the unspoken truths about RTM is it often makes visible the work you’ve already been doing informally: checking in on exercise adherence, coaching movement at a distance, or adjusting care plans between visits. In the framework of RTM as a billable service, Medicare expects you to tie that work to specific, auditable clinical intent.
So if your team still thinks RTM is “just messaging patients,” or copy-pasting some granular data, here’s a gut check: that’s not enough for Medicare. The codes are tied to:
1) data transmission via FDA-defined medical devices
2) documented need , result and outcome of the data
3) documented professional interpretation AND conveyance of the data to the patient and therapy team
Compliance Isn’t the Villain — It’s the Filter
Let’s talk about the word everyone avoids: audit.
CMS and the HHS Office of Inspector General (OIG) have both identified remote monitoring as an area of interest due to inconsistent documentation and unclear medical necessity across providers.Source: HHS Office of Inspector General – oig.hhs.gov
What’s important is what audits actually focus on.
Not volume.Not device counts.Not even minutes alone.
Auditors ask:
Why was RTM initiated for this patient?
What data was reviewed?
How did it influence clinical decisions?
Would another clinician understand the care logic?
Clinics that answer these questions clearly will pass the sniff test. Clinics that can’t… won’t.
Compliance isn’t a punishment. It’s a sorting mechanism.
RTM Platforms Don’t Fail — Processes Do
Another persistent myth in RTM is that success depends on the technology.
CMS doesn’t reimburse platforms. CMS reimburses clinically delivered services.
Findings consistently show that successful RTM programs share common traits:
defined patient selection criteria
standardized documentation language
clear roles for who reviews data and when
integration into the plan of care
Clinics that struggle often treat RTM as optional, ad-hoc, or delegated without oversight.
Technology doesn’t fix that. Process does.
RTM in 2026: Permanent, but No Longer Forgiving
CMS is not retreating from RTM. The 2026 rule changes signal the opposite: RTM is being embedded more deeply into standard care delivery models.
Expanded billing options reflect real-world care patterns—but with that flexibility comes expectation. RTM is no longer something to “try out” casually. It is expected to function as a defined, defensible pathway of care. Source: CMS – CY 2026 Medicare Physician Fee Schedule Final Rule (cms.gov)
You can still bill RTM in 2026.Just don’t expect “because we could” to hold up as a clinical rationale.
Final Thought: RTM Is a Mirror, Not a Shortcut
RTM doesn’t magically improve care. It reflects how care is already being (maybe should be?) delivered.
With the correct intention, processes, and clinical decision much of the care you provide outside of the "traditional" billable time actually becomes....billable!
For some clinics, that reflection shows intentional monitoring, engaged patients, and defensible documentation. For others, it’s a wake-up call.
Either way, if you engage in RTM in 2026, the mirror is no longer optional.
I'd love to hear how your team is engaging in RTM. Schedule a time to ensure your RTM service is on par with CMS expectations (no charge, no pressure for our first meeting).









Comments